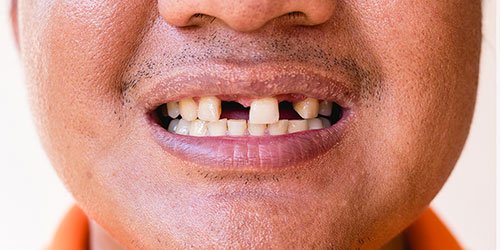
Dental implants and dentures are often used to replace missing teeth. However, restoring your smile with these techniques requires a solid, strong jawbone. If your jawbone has deteriorated since you lost a tooth, a jawbone graft can help replace some of the missing bulk, providing enough support for your replacement implant, bridge, or denture.

What is a jawbone graft?
Jawbone grafting is a surgical procedure in which bone material (organic or synthetic) is placed into the jawbone to help fill in deteriorated areas. Trauma, tooth loss, and joint issues can all lead to bone deterioration, creating an unstable foundation for tooth implants and prosthetics. Bone grafts add density and volume to areas where bone loss has occurred. Most types encourage new bone to grow, eventually integrating with the graft site.
Why would I need a jawbone graft?
When you chew, stimulation travels from your teeth into your jawbone, helping to maintain its health. Tooth loss or tooth extraction halts stimulation, and as a result, your jawbone begins to deteriorate and shrink. Implants rely on screw anchors that fasten into the jawbone, which helps restores your smile while also stimulating the bone.
However, a dental implant requires some remaining bone mass in your jaw. If you don’t have enough jawbone for an implant or prosthetic, your oral surgeon may recommend a jawbone graft to help bulk up the area. Bone grafting can also be used during ridge augmentation and sinus lift surgeries.
Types of bone grafts
Depending on your unique needs, your dentist may use one of several bone grafts. Your periodontist will recommend the best type of bone graft for your bone loss needs and restoration goals.
Properties of bone grafts
Bone grafts use one or more of the three biological healing mechanisms. Grafts that have all three generally elicit the best results. The three types of bone graft healing include:
- Osteoconductive. The bone graft serves as scaffolding, providing structure for existing bone to grow on the surface of the graft.
- Osteoinductive. Instead of acting as a prop, the bone graft material stimulates new bone growth. It actively draws in special cells called mesenchymal cells, that encourage new bone to begin forming where the graft was placed.
- Osteogenic. The bone graft contains living and viable mesenchymal stem cells, osteoblasts, and osteocytes leading to new bone formation.
Each bone graft will rely on one or more healing properties to help restabilize your jawbone before dental restoration treatments.
Dental bone graft materials
There are synthetic and organic bone graft materials, each coming from various sources.
- Autograft. An autogenous bone graft uses your bone tissue. A piece of bone is taken from one area of your body and transferred to another. In periodontal dentistry, the graft is placed within the jaw. Common places bone may be taken from include the back portion of the jaw, the chin, or even a hip. An autograft is often the preferred choice because using bone tissue from your body decreases the chance of rejection or disease. Additionally, your bone tissue uses all three growth factors to encourage healing and new bone formation, resulting in the best success rates compared to different bone grafts.
- Allograft. Alternatively, an allograft uses human bone from a donor, typically a cadaver. Natural bone is still preferable to synthetic bone, though there is a chance of disease transmission from donor bone graft material. Unlike using your bone tissue, donor bone does not contain living bone cells and only has osteoconductive and osteoinductive properties. Nevertheless, it can help promote bone regeneration.
- Xenograft. A xenograft may be the next best option if your own or donor bone cannot be used. It consists of natural bone material from a non-human source, such as bovine or porcine. These bone substitutes can act as an osteoconductive filler for the bone formation site, encouraging new bone growth.
- Synthetic (Alloplast). Synthetic materials can also be used for jawbone grafting materials. They are biocompatible and, as they are inorganic, can eliminate the risk of transmitting disease. However, synthetic dental bone graft materials don’t stimulate bone growth and generally work best as a filler rather than support for an implant. Additionally, synthetic bone has a prolonged resorption rate, sometimes not integrating well with your existing bone. Examples of synthetic materials include demineralized bone matrix or freeze-dried bone. These materials come in powder, putty, chips, or gel that consists of collagen, proteins, and growth factors extracted from allograft bone.
What is the best dental bone graft material?
Our periodontists will assess your existing bone quality and quantity, the type of surgical procedure needed, and any concerns you may have when evaluating which dental grafting material might be best. All bone graft materials used in dentistry provide volume and density to areas of bone loss. However, some provide scaffolding and new growth stimulation, with bone replacement being the ultimate goal.
For implant oral surgery, autograft bone is usually ideal. It is easily resorbable by your body, has all three bone growth stimulation characteristics, and has the lowest risk of rejection or disease transmission. Allograft and xenograft are the next best options because they are natural bones. However, these materials aren’t always available or desirable.
Synthetic bone for dental graft surgery is widely available, but it isn’t well suited to every type of oral health restoration. These materials don’t require a bone harvesting procedure, like an autograft, and therefore can cause less pain and recovery. Still, they’re best suited to procedures such as filler for beneath a bridge and not for support in an implant placement site, as healing can be unpredictable, and resorption can take years.
MD Periodontics: your partners in oral health
Dr. Abdy Moshrefi and Dr. Nazanin Daneshman are a husband-and-wife team of board-certified periodontists and holistic dentists experienced with dental grafts and the procedures they can help with, including dental implants.
Their Beverly Hills periodontology clinic aims to provide a relaxing and supportive environment for their patients. Advanced technology, excellent training, a soft bedside manner, and a stylish environment will make oral care a pleasure, not an obligation.
Schedule a consultation online or call us at (310) 859-9449. A spa-like atmosphere, staffed by a team who truly cares about your smile, awaits you!
MD Periodontics is conveniently located for patients throughout the metropolitan Los Angeles area. Our board-certified periodontists and implant dentistry experts are available at locations in or near Beverly Hills, Santa Monica, West Los Angeles, Culver City, West Hollywood, Downtown Los Angeles, Marina del Rey, Pacific Palisades, Malibu, Manhattan Beach, Sherman Oaks, and Encino.
- The Best and Worst Habits for Your Teeth - November 7, 2024
- Are cavities contagious?- September 23, 2024
- The Differences Between Dental Bone Graft Materials - September 9, 2024
 (310) 859-9449
(310) 859-9449 The Differences Between Dental Bone Graft Materials
The Differences Between Dental Bone Graft Materials 
 or call us at
or call us at