What causes dry mouth?
The dry mouth epidemic is a reality. Millions of Americans suffer from dry mouth, also known as xerostomia. Dry mouth is a medical condition that can be chronic or occur at infrequent intervals.
Dry mouth is a common side effect of over 500 different medications — including antihistamines (both prescription and over-the-counter), hypertension (high blood pressure) medications, decongestants, pain medications, diuretics, and antidepressants.
It is also commonly associated with autoimmune disorders such as Sjogren’s syndrome, HIV/AIDS, Parkinson’s disease, diabetes, hemodialysis, and radiotherapy of the head and neck region due to cancer.
To make matters worse, it’s also part of the natural aging process. While counterintuitive, it’s actually not due to a decrease in saliva production. As we age, the chemistry of the saliva changes and it becomes thicker and less able to protect the teeth and gums.

What is the function of saliva?
Saliva is produced in the salivary glands and released into the mouth via salivary ducts. There are three major salivary glands in the human body:
- Parotid gland – located near the upper teeth
- Submandibular gland – located under the tongue
- Sublingual gland – located on the floor of the mouth
Healthy saliva is a complex fluid consisting of 99% water. The remaining 1% is a mixture of proteins, enzymes, and buffering compounds (which maintain a stable pH, neutralizing small amounts of added acid or base).
Saliva is a part of the digestive process and also protects your oral health. Enzymes in the saliva break down dietary starches into simple sugars and are involved in fat digestion. It also contributes to the taste of food.
Saliva also contains proteins and minerals that protect tooth enamel and prevent tooth decay and gum disease.
Healthy adults produce between a liter and a liter and a half of saliva per day. Saliva acts as a lubricant making it easier to talk, chew, and swallow. Chewing lubricates food, forming a cohesive mass known as a bolus, allowing for passage into the esophagus.
What are the symptoms of dry mouth?
A variety of symptoms can indicate ongoing or progressing dry mouth issues. Symptoms are subjective but may be indicative of a disorder, disease, or other quality of life issue.
Usually, patients report multiple, subjective, vague symptoms. Symptoms can vary by patient and may include:
- Soreness in the mucosal lining (soft inner lining of the mouth)
- Stickiness
- Sore or dry throat
- Perceived reduction of saliva
- Hoarseness.
- Halitosis (bad breath)
- Difficulty talking, chewing, or swallowing
- Frequent thirst
- Dry mouth at night leading to poor sleep quality
- Frequent nighttime urination due to drinking for thirst relief
- Difficulty wearing dentures
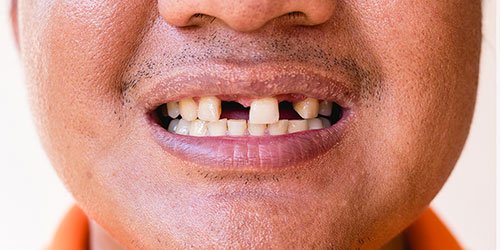
Dry mouth can also decrease or alter the sense of taste. Patients report sensitivity to salty, acidic, or spicy foods. Tooth sensitivity or recurrent decay can also be an indicator of insufficient saliva production. Patients may need to chew gum, candy, or lozenges throughout the day to moisten the oral cavity. However, this may exacerbate the problem as all three may contain sugar, increasing the chance of tooth decay.
Dry mouth usually isn’t reported until there is a perceptible reduction in salivary flow. Additionally, the early stages of dry mouth may not be recognized during a visual inspection or identified when talking to a patient.
Who suffers from dry mouth? Are there dry mouth remedies?
Dry mouth can affect people of any age, but research has demonstrated it’s predominantly a geriatric issue. Studies have shown that dry mouth affects about 30% of the population, with the number doubling for those over the age of 65. One study found that 10% of subjects in their early thirties were affected by xerostomia. And numerous studies have demonstrated that women have higher rates of dry mouth than men.

Dry mouth has a profound effect on oral homeostasis necessary for optimal dental health. Nursing home residents with and without dentures have an increased chance of a lower quality of life directly related to oral dryness — especially those with cognitive disorders like Alzheimer’s disease.
Your dentist may recommend more frequent oral hygiene visits to keep the gums and teeth healthy. Recommendations may also include brushing with fluoride toothpaste, using a fluoride rinse, drinking plenty of water, and using saliva substitutes.
What is salivary flow rate?
Salivary glands contribute to the total amount of saliva in your mouth. Each gland plays a unique role in salivary production and composition; there are also different types of salivary flow rates. The primary stimulants for saliva secretion and saliva flow are chewing, anticipatory tongue and lip movements, smell, and taste.
Evidence points to the importance of clinical assessment of oral dryness, which is a significant predictor of decreasing salivary gland function. Clinicians evaluate the following:

- Salivary production
- Flow rate
- Viscosity (state of being thick or sticky)
- pH (a measure of how acidic/basic the saliva is)
- Buffering capacity
The testing provides initial baseline data that can be used to demonstrate salivary stability and measure changes over time.
Why is decreased salivary flow bad?
Insufficient flow of saliva from the salivary glands, or hyposalivation, is a condition with numerous causes. Oral dryness creates and sustains an acidic environment that favors the growth of bacteria.
An increase in the number of bacteria in the mouth causes dental caries (tooth decay). A common fungal organism, Candida albicans, favors a highly acidic environment. Therefore, patients with dry mouth are at increased risk for oral candidiasis infections; C. albicans is also associated with periodontal disease.
Erosion is defined as the loss of hard tooth structure caused by the breakdown of minerals in an acidic environment. The breakdown of minerals causes hypersensitivity of the teeth. Both are fueled by dietary factors and are exacerbated by dry mouth.
Patients with dry mouth require careful management by dental professionals, especially if they have cognitive issues. Seniors are at the highest risk because of the prevalence of one or more diseases and taking multiple medications, both of which can cause dry mouth.
There are many contemporary lifestyle choices and environments that contribute to dry mouth. Substantial scientific evidence demonstrates how dry mouth contributes to many dental conditions, including dental caries, erosion, hypersensitivity, and fungal infections.
A strong scientific explanation for the presence of dry mouth has allowed for the development of tools necessary for the prevention, diagnosis, minimization, and reversal of the effects of this modern-day condition.
Worried about dry mouth? Talk to MD Periodontics!
MD Periodontal is the premier periodontal facility for high-quality dental care. Located in Beverly Hills, we provide a wide range of dental services. Our patients are not only local but come to us from around the globe.
Our two board-certified periodontists and their highly qualified, dedicated, and professional staff form a team that provides top-of-the-line technology and skills earned from extensive experience for you to have the best smile as well as the best oral health.
Schedule a consultation online or call us at (310) 859-9449. A spa-like atmosphere, staffed by a team who truly cares about your smile, awaits you!
MD Periodontics is conveniently located for patients throughout the metropolitan Los Angeles area. Our board-certified periodontists and implant dentistry experts are available at locations in or near Beverly Hills, Santa Monica, West Los Angeles, Culver City, West Hollywood, Downtown Los Angeles, Marina del Rey, Pacific Palisades, Malibu, Manhattan Beach, Sherman Oaks, and Encino.
- How to Care for Dental Implants: Advice From the Professionals - June 25, 2024
- The Surprising Link between Diabetes and Gum Disease - May 17, 2024
- The Power of MD Perio’s 3D Dental Scanner Workflow - April 15, 2024
 (310) 859-9449
(310) 859-9449 What is Causing The “Dry Mouth Epidemic”?
What is Causing The “Dry Mouth Epidemic”?
 or call us at
or call us at