Peri-implantitis is an inflammatory condition that affects the tissue surrounding dental implants which have replaced extracted or missing teeth. Peri-implant disease occurs when the soft tissue around a dental implant becomes infected and begins to break down. This can lead to pain, swelling, difficulty biting and chewing, and — if left untreated — implant failure.
Peri-implantitis is typically caused by poor oral hygiene and can be treated with a combination of deep cleaning and antimicrobial therapy. In severe cases, the implant may need to be removed and replaced.

What is peri-implant mucositis?
The early stage of peri-implant disease, peri-implant mucositis is similar to gingivitis (the early stage of gum disease). This early-stage infection is easier to treat than more advanced peri-implantitis and is also easily prevented through proper oral hygiene and regular dental cleanings.
Be aware, however, that oral implants are less resistant than natural teeth to the natural erosion caused by biofilm buildup. So, it is still important to prevent the development of peri-implant and periodontal diseases to keep your artificial and natural teeth healthy and in place.
How common is peri-implantitis?
The prevalence of peri-implantitis varies depending on which population you’re studying and how you define “peri-implantitis.” But overall, the prevalence of peri-implantitis is around 20%, with the highest rates being seen in people who smoke, have underlying medical conditions such as diabetes, or had a doctor who was maybe not as thorough as they could have been.
It is worth noting that the prevalence of peri-implantitis may be higher in people who have had dental implants for many years, as the risk of developing the condition tends to increase over time.
What causes peri-implantitis?
Peri-implantitis is typically caused by poor oral health, which allows bacteria to build up below the gumline. Unchecked oral bacteria can lead to infection and inflammation of the gingiva (gum tissue) and/or mucosa.
Other risk factors that we know increase the risk of developing peri-implantitis include:
- Smoking: Smokers have a higher risk of developing peri-implantitis due to decreased blood flow to the gums. Patients who smoke also have more bacterial plaque buildup in their mouths.
- Diabetes: People with uncontrolled diabetes have an increased risk of developing peri-implantitis due to decreased blood flow. Poor blood circulation hinders your ability to heal from injury or infection.
- Suppressed immune system: Immunocompromised patients — such as those with HIV/AIDS or cancer — are at higher risk of peri-implantitis. A weakened immune system cannot effectively combat the pathogens that cause periodontal disease and peri-implantitis, resulting in more severe infection.
- Poor implant placement: Improperly placed implants or implants placed in areas with insufficient bone support increase the risk of bacterial infection in peri-implant tissue.
- Overloading: Placing too much force on the implant, such as by biting or chewing on hard foods, can lead to peri-implantitis as it causes accelerated wear and damage to the implant. Tiny cracks in an implant create hiding places for bacteria.
- Poorly fitting crowns or other restorations: If a crown or other restoration does not fit properly, it can cause irritation and inflammation in the tissue at the implant site, leading to peri-implantitis.
- Skipping follow-ups: Your periodontist or dentist will want to see you for at least one follow-up appointment after dental implant treatment. At this visit, they will check for any problems with the implant or surrounding tissue. Skipping your follow-up could allow small problems to grow unchecked and become bigger problems.
What are the signs of peri-implantitis?
Symptoms of peri-implantitis may include:
- Swelling or redness of the gums around the implant.
- Discharge of pus from around the implant (suppuration).
- Pain or tenderness in the gums around the implant.
- A bad taste in the mouth.
- Loosening of the implant.
- Advanced peri-implantitis may result in lesions or bone loss.
What are peri-implantitis stages?
There are several stages of peri-implantitis. They are:
Initial inflammation
This is the earliest stage of peri-implantitis, in which the gums around the implant become red and swollen. This is often caused by bacteria that have accumulated on the implant surface.

Progressive inflammation
In this stage, the inflammation around the implant becomes more severe and can lead to the loss of bone around the implant. The gums may also become more swollen and painful.
Advanced peri-implantitis
In this stage, the inflammation and bone loss around the implant are more severe. The implant may become loose and there may be visible signs of infection, such as pus.
Failure
If peri-implantitis is not treated, the implant can eventually fail. At this point, the implant must be completely removed and bone regeneration or grafting will be required before implant therapy can be attempted again.
If caught early, we can avoid major damage and save the implant. Proper management of peri-implantitis requires intervention by a periodontal expert.
Your periodontist has access to more advanced diagnostic tools (such as radiographs) to evaluate the progression of your peri-implantitis.
Is peri-implantitis reversible?
While it is possible to treat peri-implantitis and stop the progression of the disease, it is not always reversible. The success of treatment for peri-implantitis depends on the severity of the disease and how early you begin treatment.
In the early stages of peri-implantitis, it is often possible to reverse the damage through a combination of scaling and root planing (a type of deep cleaning) and the use of antimicrobial mouthwashes or gels. If the disease is more advanced, additional treatment may be necessary, such as surgical therapy to remove infected tissue or bone grafting to treat bone loss.
What are peri-implantitis treatments?
Treatment for peri-implantitis typically involves a combination of mechanical debridement (removal of damaged tissue and bacteria) and antimicrobial therapy. The goal of these treatment options is decontamination of the tissue around the implant before the infection spreads to the jawbone.
Mechanical debridement involves removing plaque and tartar from the implant surface and surrounding tissue using specialized instruments. A periodontist can do this in their office.
Antimicrobial therapy involves using antimicrobial mouth rinses or topical gels to kill bacteria and control the infection. Chlorhexidine gluconate is a commonly used antimicrobial rinse for treating peri-implantitis.

If the peri-implantitis is severe or does not respond to non-surgical treatment, surgical intervention may be necessary. Surgical treatment for peri-implantitis may involve the removal of infected tissue and bone, as well as the placement of antimicrobial agents to help control the infection.
The Waterlase laser, which we use in our practice, is FDA-approved for the treatment of peri-implantitis. The Waterlase laser is a dental laser that combines water and laser energy. One of the benefits of using the Waterlase laser is that it can reduce the need for anesthetic (pain-relieving medication) while causing less trauma to the surrounding tissues compared to traditional dental drills.
How to prevent peri-implantitis?
Proper case planning before an implant is ever placed is extremely important for successful implant outcomes. Meaning, if you choose a doctor with a great reputation, who truly knows what they are doing, it can greatly reduce most potential issues in the first place. It’s really that simple.
How to treat peri-implantitis at home
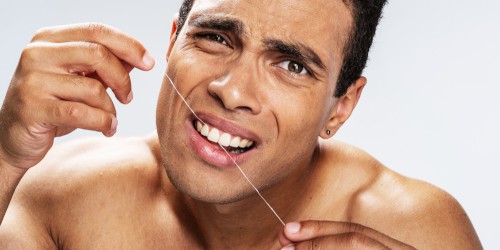
It is critically important to maintain good oral hygiene to prevent the occurrence (or reoccurrence) of peri-implantitis. Home treatment includes brushing the teeth and implant surfaces twice daily and flossing daily for effective plaque control. Also, use an antimicrobial mouthwash to remove bacteria hiding out in the mouth.
It is also important to see a periodontist regularly for cleanings and check-ups.
Worried about peri-implantitis? MD Periodontics is here to help!
You can count on two of the most respected periodontists in Southern California to help you! Dr. Abdy Moshrefi and Dr. Nazanin Daneshman are a husband-and-wife team of board-certified periodontists and holistic dentists.
At their Beverly Hills periodontology clinic, they aim to provide a relaxing and supportive environment for their patients. Advanced technology, excellent training, a soft bedside manner, and a stylish environment will make oral care a pleasure, not an obligation.
Schedule a consultation online or call us at (310) 859-9449. A spa-like atmosphere, staffed by a team who truly cares about your smile, awaits you!
MD Periodontics is conveniently located for patients throughout the metropolitan Los Angeles area. Our board-certified periodontists and implant dentistry experts are available at locations in or near Beverly Hills, Santa Monica, West Los Angeles, Culver City, West Hollywood, Downtown Los Angeles, Marina del Rey, Pacific Palisades, Malibu, Manhattan Beach, Sherman Oaks, and Encino.
Sources
Leonhardt A, Dahlén G, Renvert S: Five-year clinical, microbiological, and radiological outcome following treatment of peri-implantitis in man. J Periodontol. 2003, 74: 1415-1422. 10.1902/jop.2003.74.10.1415.
Mombelli A, Muller N, Cionca N: The epidemiology of peri-implantitis. Clin Oral Implants Res. 2012, 23 (Suppl 6): 67-76.
Zitzmann NU, Berglundh T: Definition and prevalence of peri-implant diseases. J Clin Periodontol. 2008, 35: 286-291.
- How To Pick The Best Dental Implant Specialist Near Me - September 17, 2024
- Can Bleeding Gums Be a Symptom of Something More Serious? - May 27, 2024
- What Is Hydroxyapatite Toothpaste, and Is It Better for You? - May 1, 2024
 (310) 859-9449
(310) 859-9449 What is Peri-implantitis and What to Do About It?
What is Peri-implantitis and What to Do About It?
 or call us at
or call us at